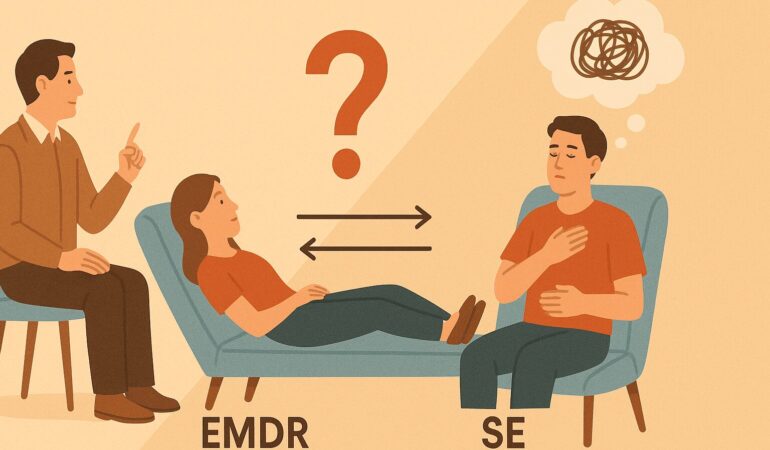
EMDR vs Somatic Experiencing: Which Helps With Trauma Triggers Faster?
Trauma can leave the body and mind reacting long after the event is over. Some people find themselves suddenly overwhelmed by flashbacks, anxiety, or physical sensations that seem to come out of nowhere. At Here Counseling, we often meet clients who ask — “Which therapy helps trauma triggers resolve faster: EMDR or Somatic Experiencing?”
Both are evidence-based trauma therapies, but they work in different ways. Understanding their differences can help you choose the approach that fits your healing process.
Understanding Trauma Triggers
Before comparing EMDR and Somatic Experiencing, it helps to understand what trauma triggers are.
A trauma trigger is anything — a sound, smell, word, or even a thought — that unconsciously reminds your body of a past traumatic experience. These triggers activate the same stress response as the original event, leading to panic, dissociation, or physical tension.
When triggers occur frequently, they can make daily life exhausting. Effective trauma therapy aims not just to manage these responses, but to reprocess the underlying memory so the body no longer perceives it as a current threat.
What Is EMDR Therapy?
Eye Movement Desensitization and Reprocessing (EMDR) is a structured, research-backed therapy designed to help people reprocess traumatic memories safely. Developed by Francine Shapiro, EMDR uses bilateral stimulation — such as eye movements, tapping, or auditory tones — while guiding you through recalling distressing experiences.
This process helps the brain move the memory from the “stuck” state in the limbic system to the rational part of the brain, where it can be processed without intense emotional charge.
Clients often describe it as being able to remember the trauma without reliving it.
What EMDR targets:
- Post-Traumatic Stress Disorder (PTSD)
- Single-event trauma (accidents, assault, disasters)
- Anxiety and panic
- Emotional distress related to specific memories
In many cases, EMDR produces noticeable relief within fewer sessions compared to talk therapy, making it a powerful choice for individuals seeking structured trauma resolution.
What Is Somatic Experiencing?
Somatic Experiencing (SE), developed by Dr. Peter Levine, focuses on how trauma is stored in the body rather than in thoughts or memories. Trauma can leave the nervous system in a constant state of fight, flight, or freeze. Somatic Experiencing helps restore balance by gently guiding the body to release stored survival energy.
Rather than revisiting traumatic memories in detail, SE works by increasing awareness of bodily sensations — tension, tightness, breath patterns — and allowing these sensations to resolve gradually.
Somatic Experiencing helps with:
- Chronic stress and burnout
- Developmental or complex trauma
- Anxiety and hypervigilance
- Physical symptoms linked to emotional distress (e.g., muscle tightness, fatigue)
Sessions are often slower-paced and body-focused, emphasizing safety and regulation.
EMDR vs Somatic Experiencing: How They Differ
Both therapies aim to reduce trauma symptoms and emotional reactivity, but they differ in focus and process.
| Aspect | EMDR | Somatic Experiencing |
| Focus | Reprocessing traumatic memories | Regulating the nervous system and releasing body-held tension |
| Approach | Uses bilateral stimulation to desensitize distressing memories | Uses body awareness to track and release trauma responses |
| Session Structure | Structured and protocol-based | Fluid and experiential |
| Ideal For | Single-event trauma or PTSD | Chronic or developmental trauma |
| Speed of Results | Often faster for specific memories | Gradual, deeper nervous system repair |
If you’re looking for quicker symptom relief, EMDR may show progress sooner, especially for identifiable traumatic events.
If your trauma is long-term or linked to ongoing stress patterns, Somatic Experiencing may be a better long-term approach.
Which Works Faster for Trauma Triggers?
The question of speed depends on the type of trauma and how your nervous system responds to treatment.
EMDR is generally faster for acute trauma — such as a car accident, loss, or assault — because it helps reprocess a specific event. Clients often notice a decrease in emotional intensity after a few sessions.
Somatic Experiencing, on the other hand, is more effective for chronic stress or complex trauma, where the body has learned to stay in a constant state of alert. The process is slower, but it creates foundational nervous system regulation, which reduces the intensity of future triggers.
In other words, EMDR tends to address the “flash” of the memory, while Somatic Experiencing addresses the body’s ongoing reaction to that flash. Many trauma-informed clinicians integrate both methods to achieve faster and deeper healing.
The Science Behind EMDR and Somatic Experiencing
Both EMDR and Somatic Experiencing are grounded in neuroscience.
- EMDR works by activating the brain’s natural reprocessing system, similar to what occurs during REM sleep. This helps integrate fragmented memories into normal narrative memory.
- Somatic Experiencing targets the autonomic nervous system — the network controlling stress responses. By releasing stored tension, SE helps restore a sense of safety and presence.
Research supports both approaches. The APA and WHO recognize EMDR as an effective trauma therapy. Somatic Experiencing is supported by emerging studies showing reductions in anxiety, PTSD symptoms, and physiological stress markers.
Choosing Between EMDR and Somatic Experiencing
Choosing a trauma therapy depends on your history, symptoms, and what feels safe for you.
At Here Counseling, we often discuss the following with clients before deciding on a treatment plan:
- Nature of the trauma: Was it a single event or repeated over time?
- Body awareness: Do you feel disconnected from your body, or overly reactive to sensations?
- Comfort level: Are you comfortable revisiting traumatic memories, or would you rather work indirectly through sensations?
- Therapy goals: Are you seeking faster symptom relief or long-term regulation?
Both methods can be effective, and sometimes combining them — for instance, using Somatic Experiencing to ground the body before EMDR — leads to better outcomes.
Can EMDR and Somatic Experiencing Be Combined?
Yes. Many trauma therapists integrate both modalities.
For example, a client might start with Somatic Experiencing to build safety and body awareness. Once their nervous system feels more regulated, EMDR can help reprocess specific traumatic memories without overwhelming the body.
This integrated approach allows for both emotional desensitization and physical release — a balance that helps reduce trauma triggers more sustainably.
The Role of the Therapist
The effectiveness of trauma therapy depends not only on the method but also on the therapeutic relationship.
At Here Counseling, our trauma-informed therapists are trained in EMDR, Somatic Experiencing, and integrative approaches. We focus on pacing sessions according to your nervous system’s readiness, ensuring you feel supported and grounded throughout your healing journey.
Every client’s trauma story is unique. Our goal isn’t just to help you cope with triggers, but to help your mind and body truly feel safe again.
When to Seek Help for Trauma Trigger
If you find yourself:
- Easily startled or anxious
- Reliving past events through flashbacks or nightmares
- Feeling detached from your body or surroundings
- Physically tense or fatigued without clear reason
you may be experiencing unresolved trauma responses.
Reaching out for help doesn’t mean your trauma defines you — it means you’re ready to take back control of your life.
How We Help at Here Counseling
Whether through EMDR therapy in Pasadena or Somatic Experiencing sessions, we help clients process trauma safely and effectively — in person or through secure online sessions.
We focus on creating a space where you can understand your triggers, regulate your nervous system, and move toward lasting emotional balance.
If you’re unsure which approach is right for you, we’ll guide you through the options, explain what to expect, and design a plan that fits your comfort level and goals.
Frequently Asked Questions
Is EMDR better than Somatic Experiencing for PTSD?
Both are effective for PTSD. EMDR is usually faster for single-event trauma, while Somatic Therapy helps with chronic or developmental trauma.
How many sessions will I need?
It varies. EMDR may bring relief in several sessions; Somatic Experiencing often requires a longer process for deep nervous system regulation.
Can I do these therapies online?
Yes. Both EMDR and Somatic Experiencing can be conducted virtually with proper therapist guidance.
Do I need to relive my trauma during EMDR?
No. You recall the event briefly but from a safe and guided state. The goal is to reprocess, not to retraumatize.
Can I combine EMDR with Somatic Experiencing?
Absolutely. Many clients benefit from integrating both to balance emotional and physical healing.
Begin Healing With Trauma Therapy in Pasadena
Healing from trauma isn’t about erasing the past — it’s about freeing your body and mind from its grip.
At Here Counseling, we offer EMDR and Somatic Experiencing therapy in Pasadena, helping you manage trauma triggers, rebuild safety, and move forward with greater calm and confidence.